Skin Cancer
Overview
Skin cancer is a common form of cancer and develops when skin cells grow and divide in an uncontrolled way. It most often appears on areas of the skin that receive frequent sun exposure, but it can form anywhere on the body, including areas not typically exposed to sunlight. The three main types are:
- Basal cell carcinoma
- Squamous cell carcinoma
- Melanoma
Melanoma is the least common but most serious type of skin cancer. It begins in melanocytes, the cells that produce melanin, the pigment that gives skin its color. While melanoma typically develops on the skin, it can also occur in the eyes and, rarely, in internal areas such as the nose or throat.
Ultraviolet (UV) radiation from sunlight or tanning beds is the primary risk factor for most skin cancers, including melanoma. Although anyone can be affected, melanoma rates have risen in people under 40, especially women. Regular skin checks, sun protection, and knowing what warning signs to look for can help detect skin cancer early, when treatment is most effective.
What Makes Melanoma Different
Melanoma begins in melanocytes, the pigment-producing cells of the skin. Unlike more common skin cancers that tend to grow slowly and stay localized, melanoma can spread more quickly if not found early.
Melanoma is more aggressive because abnormal melanocytes can invade deeper layers of the skin and enter the bloodstream or lymphatic system sooner than other skin cancer types.
While UV exposure is a major driver, melanoma also develops when genetic changes (mutations) inside melanocytes cause them to grow uncontrollably. These changes can be triggered by sun exposure, tanning beds, or occur without an obvious cause.
Early detection is crucial. When melanoma is found and treated at its earliest stage, outcomes are excellent. Monitoring your skin regularly and knowing what to look for can make a significant difference.
ABCDE Rule
ABCDE rule is a simple way to identify moles or spots that may be concerning for melanoma. This tool helps you recognize changes that should be evaluated by a healthcare professional.
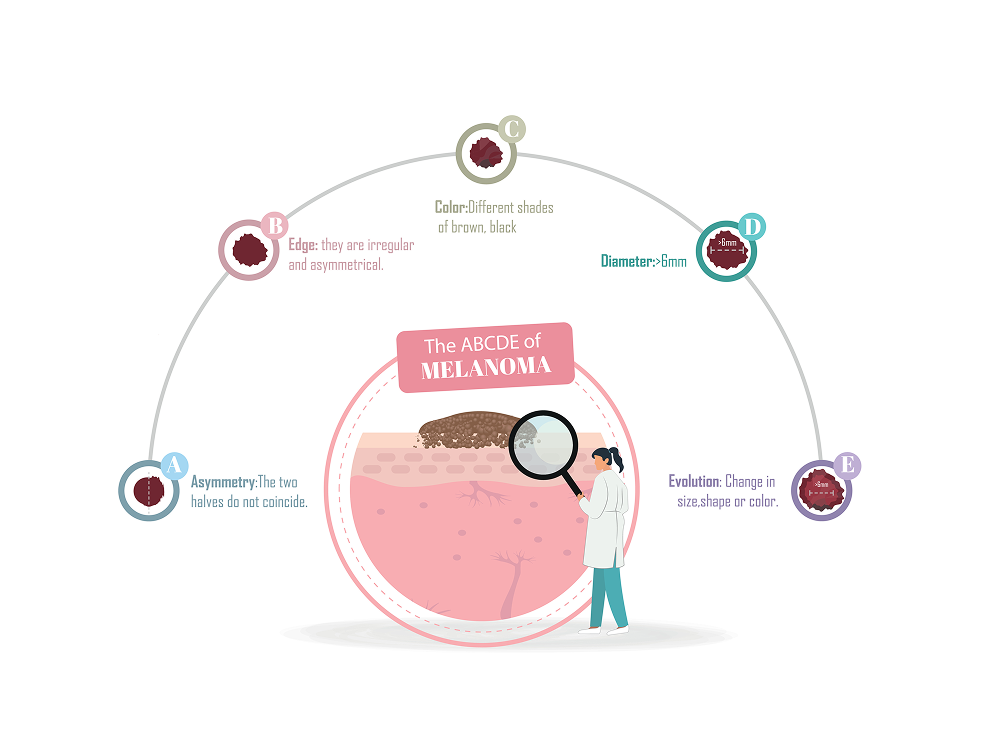
A — Asymmetry: One half of the mole doesn’t match the other.
B — Border: Edges are irregular, blurred, or uneven.
C — Color: Multiple colors or shades within the same spot.
D — Diameter: Larger than 6 millimeters (about the size of a pencil eraser), though melanoma can be smaller.
E — Evolving: Any change in size, shape, color, or symptoms like itching or bleeding.
If you notice any of these features, or if a spot simply looks different from others (“the ugly duckling sign”), it’s important to get it checked promptly. Early evaluation leads to the best outcomes.
Signs & Symptoms
Skin cancer can appear anywhere on the body, though it most often develops in areas that receive frequent sun exposure such as the face, neck, chest, arms, hands, and legs. It can also form in areas that rarely see sunlight, including the scalp, palms, soles, under nails, and the genital region. Skin cancer affects people of all skin tones. In individuals with darker skin, cancers, especially melanoma, are more likely to appear on the palms, soles, or under the nails.
| Type of Skin Cancer | Signs & Symptoms |
|---|---|
| Basal Cell Carcinoma: most common type of skin cancer and typically appears on sun-exposed areas such as face, ears, or neck. | A pearly, waxy, or translucent bump. A flat, flesh-colored or slightly brown scar-like patch. A sore that bleeds, crusts, and repeatedly returns. |
| Squamous Cell Carcinoma: often develops on sun-exposed skin like the face, ears, scalp, or hands. In people with darker skin, it may appear in areas not typically exposed to the sun. | A firm, red or pink nodule. A flat lesion with a scaly, crusted surface. |
| Melanoma: can form anywhere; in an existing mole or on previously normal-appearing skin. It is more common on the back, chest, or face in men and on the legs in women. In people with darker skin, melanoma more often appears on the palms, soles, or under the nails. |
A large brown spot with darker speckles. A mole that changes in size, shape, color, or begins to bleed. A small, irregular lesion with varying colors. A painful, itchy, or burning spot. Dark lesions on the palms, soles, fingertips, toes, or mucous membranes.
|
| Less Common Skin Cancer - Kaposi Sarcoma | Causes red or purple patches on the skin or mucous membranes. More common in people with weakened immune systems or certain inherited backgrounds. |
| Less Common Skin Cancer - Merkel Cell Carcinoma | Presents as fast-growing, firm, shiny nodules on the head, neck, or trunk. |
| Less Common Skin Cancer - Sebaceous Gland Carcinoma | A rare, aggressive cancer often appearing as a hard, painless nodule, most commonly on the eyelid and easily mistaken for a benign eyelid condition. |
Causes of Skin Cancer and Melanoma
Skin cancer develops when the DNA inside skin cells becomes damaged and the cells begin to grow and divide in an uncontrolled way. Over time, these abnormal cells can form a tumor and, in some cases, spread to other parts of the body.
Most skin cancers begin in the upper layer of the skin (the epidermis), which contains three main types of cells:
- Basal cells, which create new skin cells
- Squamous cells, which form the inner lining of the skin
- Melanocytes, which produce melanin, the pigment that gives skin its color
Where the cancer starts helps determine its type and treatment approach.
For many people, the primary source of DNA damage is ultraviolet (UV) radiation from the sun or from tanning beds. UV rays can harm skin cells quickly, and repeated exposure overwhelms the body’s ability to repair that damage. Over time, this increases the risk of all major skin cancers, basal cell carcinoma, squamous cell carcinoma, and melanoma.
Melanoma forms when melanocytes, the pigment-producing cells, develop DNA changes that cause them to grow out of control. UV exposure is the leading cause of this damage, but it’s not the only one. Melanomas can also occur in places with little or no sun exposure, showing that genetic changes, immune function, and other environmental factors can also play a role.
Not all skin cancers are caused by UV radiation. Additional factors that can contribute include:
- Exposure to certain chemicals or carcinogens
- A weakened immune system
- Chronic inflammation or repeated skin injury
Together, these factors can disrupt the normal life cycle of skin cells and lead to cancer formation.
Risk Factors
A number of factors can increase the risk of developing skin cancer, including melanoma. While anyone can be affected, some people have characteristics or exposures that make skin cancers more likely to form. Common risk factors include:
- Fair or light skin: People with less melanin have less natural protection from UV damage. Individuals with blond or red hair, light eyes, or skin that freckles or burns easily are at higher risk, though skin cancer can occur in any skin tone.
- History of sunburns: Severe or blistering sunburns, especially in childhood or adolescence, significantly increase lifetime risk. Repeated sunburns in adulthood also raise risk.
- Excessive UV exposure: Spending long periods in the sun without protection or using tanning beds increases the risk of basal cell carcinoma, squamous cell carcinoma, and melanoma. A tan is a sign of skin injury, not health.
- Living in sunny or high-altitude climates: More direct sunlight and thinner atmospheric protection increase exposure to UV radiation, even during cooler months.
- Having many moles or atypical moles: A large number of normal moles, especially more than 50, increases melanoma risk. Atypical or dysplastic moles (larger, irregular, or multicolored) carry an even higher chance of becoming cancerous.
- Precancerous skin lesions: Actinic keratoses, rough scaly patches caused by long-term sun exposure, can progress to skin cancer if left untreated.
- Family history of skin cancer or melanoma: Having a close relative with skin cancer increases your risk, especially for melanoma.
- Personal history of skin cancer: If you’ve had skin cancer once, you are more likely to develop it again.
- A weakened immune system: Conditions like HIV/AIDS, or medications that suppress the immune system after organ transplant, increase the risk of all forms of skin cancer.
- Past radiation exposure: Prior radiation therapy, even years earlier, can increase the likelihood of developing basal cell carcinoma.
- Exposure to certain chemicals: Contact with substances such as arsenic can raise the risk of skin cancer.
Preventing Skin Cancer
Protecting your skin from ultraviolet (UV) radiation is the most important way to lower your risk of skin cancer, including melanoma. Limit sun exposure when UV rays are strongest, typically between 10 a.m. and 4 p.m., even on cloudy or cold days. Use a broad-spectrum SPF 30+ sunscreen, apply generously, and reapply every two hours or after swimming or sweating. Wearing tightly woven clothing, a wide-brimmed hat, and UV-blocking sunglasses provides additional protection.
Tanning beds and sunlamps emit concentrated UV radiation that damages skin cells and raises the risk of all forms of skin cancer. Avoiding indoor tanning entirely is one of the best ways to reduce long-term risk.
Regular skin self-exams help you notice new or changing spots early. Look for changes in moles, freckles, or new growths using mirrors to check your scalp, back, feet, and other hard-to-see areas. Report any changes to a clinician promptly; early detection dramatically improves outcomes, especially for melanoma.
UV damage occurs year-round, even during winter or when skies are overcast. People living at high altitudes or near the equator receive more intense UV exposure. Some medications, including certain antibiotics, can make the skin more sensitive to sunlight. If your medications increase UV sensitivity, take extra precautions outdoors.
Certain factors, such as fair skin, a personal or family history of skin cancer, many or atypical moles, or a weakened immune system, increase your risk. If you have higher-than-average risk, talk with your doctor about how often you should have professional skin exams.
Diagnosing Skin Cancer
Evaluation begins with a detailed skin exam. A clinician assesses any spots, moles, or lesions that appear unusual, have changed over time, or meet criteria such as the ABCDEs of melanoma.
A dermatoscope, a handheld device that magnifies and illuminates the skin, helps clinicians see structures beneath the surface. Dermoscopy improves detection of early skin cancers and helps differentiate benign moles from suspicious lesions.
If a lesion appears concerning, part or all of it is removed for microscopic evaluation. Techniques may include shave biopsy, punch biopsy, or excisional biopsy depending on the location and type of lesion. A biopsy is the only definitive way to diagnose skin cancer and determine the specific type.
When melanoma is diagnosed, further testing may be recommended to understand the extent of disease. This may include:
- Sentinel lymph node biopsy to determine if melanoma has spread to nearby lymph nodes
- Imaging tests, such as CT or PET scans, for more advanced or higher-risk melanomas
- Tumor thickness and ulceration assessment, which help guide treatment decisions
Stage is assigned using Roman numerals (0–IV), based on tumor depth, lymph node involvement, and spread to other organs. Early-stage melanomas often require surgical removal alone, while more advanced disease may need additional therapy.
Treatments & Services
Treatment Options
Treatment depends on the type of skin cancer, how advanced it is, and where it appears on the body. Your care team will tailor a plan that prioritizes removing the cancer, protecting healthy tissue, and supporting long-term skin health.
For melanoma, additional systemic therapies or lymph node evaluation may be recommended based on the stage and molecular profile of the tumor.
Service Options
Find Care
Our specialists diagnose and treat all forms of skin cancer, from common to complex. Find your nearest location to connect with a care team dedicated to providing personalized, evidence-based treatment and ongoing support.
Our Locations
We offer locations across the DFW metroplex so you can receive leading cancer care and support close to home.
Our Care Team
Get to know the compassionate experts who guide your care with a whole-person approach—spirit, mind, and body.
Request an Appointment
Contact us to request an appointment or ask a question below. For emergencies call 911 or visit your nearest hospital.